To help our readers keep track of the cancer therapies approved by the U.S. Food and Drug Administration (FDA), understand their impact for patients, and put them in context of the current therapeutic landscape, Cancer Research Catalyst provides a quarterly review of the latest approvals in oncology from the FDA.
From April 1 to June 30, 2025, the U.S. Food and Drug Administration (FDA) issued 13 new oncology approvals, expanding treatment options for patients with a variety of cancers. Notably, these approvals included several therapeutics new to the market, as well as new treatment options for patients with rare diseases.
For the First Time in Decades, A New Treatment Option for Locally Advanced Head and Neck Cancer
For more than 20 years, the standard treatment for locally advanced head and neck cancers has been surgery followed by radiation therapy with or without chemotherapy, but an FDA approval issued this quarter provides a potential new standard of care.
- Perioperative pembrolizumab (Keytruda), an immune checkpoint inhibitor, was approved for the first-line treatment of adult patients with resectable, locally advanced, PD-L1-positive head and neck squamous cell carcinoma (HNSCC). The approval requires that pembrolizumab be given as monotherapy before surgery, in combination with radiation therapy and/or chemotherapy for several weeks after surgery, and as monotherapy thereafter up to two years or until unacceptable toxicity or disease progression.
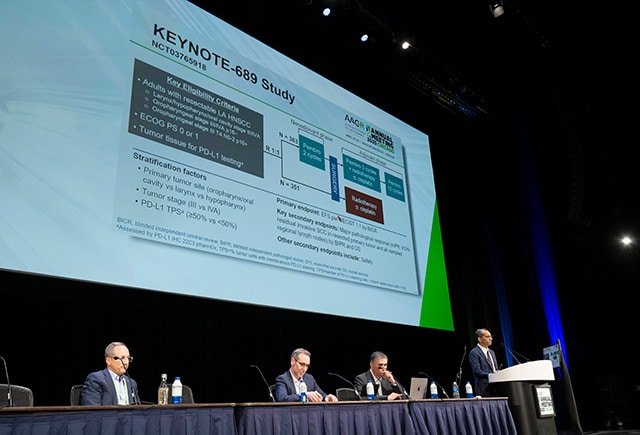
The approval was based on phase III clinical trial results first reported at the AACR Annual Meeting 2025 by Ravindra Uppaluri, MD, PhD, of the Brigham and Women’s Hospital, the Dana-Farber Brigham Cancer Center, and Harvard Medical School. During a Clinical Trial Plenary Session, Uppaluri shared that patients with PD-L1-positive HNSCC enrolled in the KEYNOTE-689 trial had a 34% lower risk of disease recurrence if they received perioperative pembrolizumab along with standard therapy.
In an AACR press release, Uppaluri noted that “this new information supports changing the current standard of care to now include neoadjuvant and adjuvant pembrolizumab. For the first time in more than 20 years, patients with this challenging disease have a new therapeutic approach.”
Check out a recent blog post to learn more about the data from the clinical trial that led to this FDA approval.
Advances in Treating Rare Cancers
Researchers face many challenges when developing and testing new treatments for rare cancers, including limited tumor samples and experimental models to study these diseases as well as few patients to enroll into clinical trials to test investigational therapeutics.
For these reasons, progress against rare cancers can be slower than for more common cancers. This quarter, however, offered some hope, with four new treatment options approved for rare cancers of the anus, nasopharynx, nervous system, and ovaries.
- The immune checkpoint inhibitor retifanlimab-dlwr (Zynyz) was approved for patients with locally recurrent or metastatic squamous cell carcinoma of the anal canal (SCAC), either
- in combination with chemotherapy as first-line treatment for patients with inoperable SCAC, or
- as a single agent for patients who have had disease progression on or intolerance to prior chemotherapy.
SCAC is the most common form of anal cancer, which accounts for just 0.5% of all cancer cases in the United States.
- Another immune checkpoint inhibitor, penpulimab-kcqx, was approved for patients with nonkeratinizing nasopharyngeal carcinoma, either
- in combination with chemotherapy for the first-line treatment of recurrent or metastatic nonkeratinizing nasopharyngeal carcinoma, or
- as a single agent for patients whose metastatic nonkeratinizing nasopharyngeal carcinoma progressed on or after platinum-based chemotherapy and at least one other line of treatment.
These represent the first FDA approvals for penpulimab-kcqx, which were based on clinical trial results reported at the AACR Annual Meeting 2025. Nasopharyngeal carcinoma is a rare type of head and neck cancer diagnosed in fewer than 1 out of every 100,000 individuals worldwide.

- The HIF1-targeted drug belzutifan (Welireg) was greenlit for the treatment of patients 12 years and older with locally advanced, unresectable, or metastatic pheochromocytoma or paraganglioma (PPGL), which are rare nerve cell cancers that occur within the adrenal gland or near blood vessels, frequently leading to high blood pressure.
Belzutifan is the first oral therapy to receive FDA approval for PPGL. In addition to inducing tumor responses, the therapeutic may allow some patients with PPGL to reduce their dose of blood pressure-controlling medications.
- The targeted therapeutics avutometinib and defactinib (Avmapki Fakzynja Co-pack) received accelerated approval to treat a rare form of ovarian cancer known as low-grade serous ovarian cancer (LGSOC), which responds poorly to chemotherapy. The approval is for KRAS-mutated LGSOC that has recurred after prior systemic therapy. This is the first FDA approval for avutometinib and defactinib, which work by inhibiting cell signaling pathways that drive cancer.
Two New Approvals for First-line Nivolumab and Ipilimumab Combination
Nivolumab (Opdivo) and ipilimumab (Yervoy) are immune checkpoint inhibitors that promote antitumor immune responses by targeting PD-1 and CTLA-4, respectively. These inhibitors are often combined to enhance their effect, and the combination has been approved for several cancer types as first-line or subsequent-line treatment.
For colorectal cancers and liver cancers, the combination was previously approved only for patients whose disease had progressed after prior treatment, but two recent approvals have made the combination available for the first-line treatment of these cancers as well.
- The nivolumab and ipilimumab combination was approved for the treatment of patients 12 years and older with unresectable or metastatic colorectal cancer characterized by mismatch repair-deficient or microsatellite instability-high (dMMR/MSI-H) status.
- The nivolumab and ipilimumab combination was also approved for the first-line treatment of unresectable or metastatic liver cancer.
New Ways to Direct Cytotoxic Drugs to Cancer Cells
Chemotherapy has long been a workhorse of cancer treatment. While effective at killing cancer cells, its widespread activity on noncancer cells throughout the body can lead to harsh side effects. Researchers, therefore, have developed strategies to more precisely direct chemotherapy and other cytotoxic drugs to cancer cells and reduce their effects on healthy tissue.
One such strategy is to link the cytotoxic drug to an antibody that recognizes cancer-associated proteins. These constructs, known as antibody-drug conjugates, deliver cytotoxic agents selectively to cells that express the target protein, which tend to be primarily cancer cells.
This quarter, the FDA approved two antibody-drug conjugates for non-small cell lung cancer (NSCLC).
- Telisotuzumab vedotin-tllv (Emrelis) was granted accelerated approval for nonsquamous NSCLC that is locally advanced or metastatic, has been previously treated with systemic therapy, and overexpresses the c-Met protein. This is the first FDA approval for telisotuzumab vedotin-tllv.
Telisotuzumab vedotin-tllv consists of a cytotoxic agent called monomethyl auristatin E linked to a c-Met targeted antibody. It is the first c-Met-targeted therapy approved to treat lung cancers that express wild-type c-Met.

- Datopotamab deruxtecan-dlnk (Datroway) received accelerated approval for patients with locally advanced or metastatic NSCLC whose cancers harbor a mutation in the epidermal growth factor receptor (EGFR) and who have received prior treatment with an EGFR-targeted therapy and chemotherapy.
This antibody-drug conjugate uses a TROP-2-directed antibody to deliver the cytotoxic agent deruxtecan to cells expressing TROP-2, a protein whose expression has been implicated in resistance to EGFR-targeted therapy.
Another strategy to more precisely deliver cell-killing agents is to administer them locally to the part of the body where the tumor is, rather than systemically. While healthy cells near the tumor are still exposed to the drug, those in other parts of the body are generally spared. An example of this approach is intravesical administration, in which therapeutics for bladder cancer are delivered directly into the bladder via a urinary catheter.
- This quarter, the FDA approved a new intravesical treatment, mitomycin intravesical solution (Zusduri), for low-grade, non-muscle invasive bladder cancer that recurred after surgery.
Mitomycin is a chemotherapy drug that is typically delivered systemically to treat other cancer types. In addition to local delivery, the newly approved formulation also encapsulates mitomycin within a hydrogel that allows for sustained drug release within the bladder.
Therapies Targeting ROS1, Androgen Receptor, and CD19
This quarter’s FDA approvals also featured therapeutics targeting cancer-promoting or cancer-associated proteins.
- The ROS1 inhibitor, taletrectinib (Ibtrozi), was approved to treat patients with locally advanced or metastatic NSCLC that harbors a fusion or rearrangement involving the ROS1 gene. These types of gene alterations are known to promote tumor development.
This is the first FDA approval for taletrectinib, which has been shown to be effective against lung cancers that harbor the G2032R ROS1 mutation, which is associated with resistance to previously approved ROS1 inhibitors.
- Darolutamide (Nubeqa) was approved for the treatment of patients with metastatic castration-sensitive prostate cancer (mCSPC). Darolutamide is an inhibitor of the androgen receptor, which, upon binding testosterone, activates signaling pathways that drive prostate cancer growth.
- A combination of tafasitamab-cxix (Monjuvi), lenalidomide (Revlimid), and rituximab (Rituxan) was approved for patients with relapsed or refractory follicular lymphoma. Tafasitamab-cxix is a monoclonal antibody that recognizes CD19, a protein expressed on normal and cancerous B cells, including follicular lymphomas. Binding of tafasitamab-cxix to CD19 leads to death of the CD19-expressing cell.
Lenalidomide is an immunomodulatory drug commonly included in treatment regimens for certain B-cell cancers. Rituximab is an antibody that targets the protein CD20 on B cells and triggers the immune system to destroy them.
Check out our FDA approvals page for a comprehensive overview of each oncology approval, including the clinical data that led to each.