From 2001 to 2021, the pediatric cancer death rate fell by 24%, but these benefits were not distributed among all pediatric cancers equally. While many children with leukemia are living significantly longer, thanks largely to advances in cell therapy, outcomes for children with cancers of the brain and central nervous system (CNS) have barely improved.
Though scientific progress has been made, brain and CNS cancers are now the leading cause of cancer-related death in children, and too often the best tools we have buy only a little time while stealing precious potential memories in the process. Parents often watch their children lose vision, balance, or even the ability to speak as aggressive tumors, and the harsh treatments used against them, take their toll.
Spurred by the success of chimeric antigen receptor (CAR) T-cell therapy in childhood leukemia, scientists now seek to use these “living drugs” to similarly shift the scale for young people with cancers of the brain and spinal cord, which come in a variety of forms and affect approximately 4,300 children each year in the United States.
As highlighted in a review in Cancer Discovery, a journal of the American Association for Cancer Research (AACR), groundbreaking clinical trials are providing early insights into the potential safety and anticancer activity of these cell therapies, while preclinical research is exploring solutions to the unique challenges facing the application of CAR T cells in children with brain and CNS cancers.
Circumventing the Blood-brain Barrier
There is only one CAR T-cell therapy currently approved for children: tisagenlecleucel (Kymriah) for acute lymphoblastic leukemia (ALL). The treatment is created by taking a patient’s own T cells and engineering them to express a receptor—the CAR—that targets a certain protein on cancer cells. In the case of leukemia, the CARs target CD19. Once equipped with CD19-targeting CARs, these enhanced T cells are multiplied into millions and then, via intravenous (IV) infusion, put back into the patient’s bloodstream where they circulate and destroy CD19-expressing leukemia cells with incredible efficiency.
But the peripheral blood has drastically different features than the privileged vault of the brain, and brain cancers have little in common with blood cancers. In leukemia, CAR T cells released into the bloodstream can roam freely to find cancer. But the brain is an entirely different arena, and the blood-brain barrier can bar circulating CAR T cells from easy entry and may hinder their ability to engage brain tumors in children or adults.
Therefore, researchers are testing intracranial (IC) delivery routes that place CAR T cells directly into the CNS via a catheter or port. Supplying the immune cells locally behind the blood-brain barrier can concentrate the attack at the tumor and, according to one study that evaluated both IV and IC delivery, may lessen the likelihood of systemic side effects like cytokine release syndrome (CRS) and immune cell-associated neurotoxicity syndrome that can follow CRS. Here, both IC and IV delivery approaches caused local tumor inflammation-associated neurotoxicity, though it did not cause any patients to discontinue therapy.
Setting the Immune System’s Sights on Central Nervous System Cancers
Another key challenge is finding good targets that enable CAR T cells to be effective against brain and CNS cancers in children. In contrast to the CD19 target expressed by essentially all leukemia cells, pediatric brain tumors have no such defining target. These tumors typically do not have many mutations either, so they express few mutant proteins that could serve as cancer-specific targets for T cells, engineered or otherwise.
There are two exceptions, though neither provides an ideal target like CD19. The first, H3 K27M, is a mutation found in the majority of pediatric cases of diffuse midline glioma, a subset of pediatric CNS tumors that includes diffuse intrinsic pontine glioma. But the H3 K27M mutation does not provide a good target because it occurs in a protein within the nucleus, rather than one on the cell surface, so it is beyond the reach of today’s CAR T cells. The second mutation, EGFRvIII, is not nearly as common in pediatric CNS tumors, but because it results in a mutated protein on the cell surface it provides a more suitable target when present. Multiple trials are evaluating CAR T cells that target mutant EGFRvIII in children and young adults with relapsed or refractory CNS cancer.

The Cancer Discovery review also highlighted trials exploring tumor-associated proteins as CAR T-cell targets. These normal proteins can be abundant on tumor cells compared to normal cells, both in the brain and elsewhere. Thus, strategies designed against them could help minimize off-target CAR T-cell activity. Two tumor-associated proteins, human epidermal growth factor receptor 2 (HER2) and GD2, already serve as the basis for non-CAR T-cell therapies approved in other cancers, and two others, B7-H3 and interleukin-13 receptor alpha 2 (IL13Ralpha2), are also under clinical investigation. Abnormal signaling in these different pathways can aid cancer cells by helping them grow or regulate immune responses that might otherwise eliminate them, among other impacts.
Initial results from the various trials offer reason for hope and cautious optimism. In particular, CAR T cells targeting GD2 have led to responses in pediatric patients, and several children with aggressive disease saw their cancers shrink and went on to live far longer than expected. Though none of the trials was substantial enough to offer anything definitive, they did show that CAR T cells can, in certain cases, trigger powerful antitumor immunity against CNS cancers in children. Immune-related side effects can occur, but through the field’s experience with CAR T cells in leukemia, doctors have learned how to better manage these problems if they arise.
Of note, a trial for children with neuroblastoma—a cancer that most often affects the peripheral, not central, nervous system—utilized GD2 CAR T cells created using donor T cells, an allogeneic approach that could overcome some of the manufacturing challenges associated with creating each patient’s therapy from their own immune cells, and hopefully improve the therapy’s cost and deliverability.
Smarter CAR T Cells and Reprogramming TIME in Pediatric CNS Tumors
To turn rare successes into more frequent outcomes, scientists are redesigning CAR T cells to be more effective against pediatric brain cancers. One focus is addressing the fact that if CAR T cells target only one protein, any cancer cell that lacks that marker can escape and regrow the tumor, a phenomenon known as antigen escape. To counter that, new CAR T cells are being built to recognize multiple targets at once. For example, one trial is testing a “quad-CAR” that can recognize four tumor-associated targets simultaneously to cast a wider net against cancer. Researchers are also adding safety features like logic gates so that engineered T cells activate only under the right conditions, attacking tumor cells while sparing healthy ones.
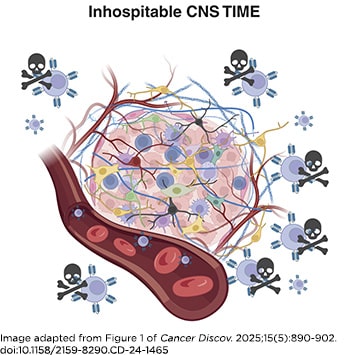
Even the best CAR T cells may falter if the tumor immune microenvironment (TIME) remains hostile. Brain tumors in children (and adults, too) often create an immunosuppressive region that hides them from immune attack or weakens T-cell responses through the signaling of cytokines like IL-10 and transforming growth factor (TGF)-beta. In the case of TGF-beta, researchers revealed that making CAR T cells resistant to its effects can enhance their antitumor activity in preclinical models of glioma.
Other strategies to improve the durability and persistence of CAR T cells in the body involve designs that equip them with an always-signaling IL-7 receptor or enable them to produce bispecific T-cell engagers that target cancer cells while rallying the body’s natural T cells. All of these tweaks aim to prevent the cancer from finding loopholes and to keep CAR T cells active against cancer longer.
Combining other therapies along with CAR T-cell therapies could also help tip the TIME balance against the tumor, including with immune checkpoint inhibitors, which can boost T-cell responses, and therapies that modify the epigenetic patterns that impact which genes cells are activated. These latter therapies can affect cancer cells directly as well as alter immune cell activity. Efforts to reshape the local tumor microenvironment in preclinical models show that such strategies might be able to help CAR T cells sustain a more durable response in patients, too.


